Mediterranean Diet Patient Education Plan for Diabetes Management

Place your patients on the Mediterranean Diet Plan to guide them through a practical heart-healthy eating plan that will help with blood sugar and diabetes management.
What is the Mediterranean Diet for Diabetes Plan?
The Mediterranean Diet for Diabetes Plan is an automated plan that will educate your patients on the basics of type 2 diabetes and heart health all while supplying your patients with the nutrients they’ll need to help manage their blood sugar. This diet is rich in raw fruits, vegetables, and only healthy fats. Imagine a splash of flavorful olive oil and perhaps even a glass of red wine.
Prescribing the Mediterranean Diet program may be a fit for patients who are trying to better control their blood sugar levels or for those looking to manage diabetes. It may also be a helpful program for those with metabolic syndrome.
Additionally, this diet also recognizes the importance of being physically active and enjoying shared meals with family and friends.
How Can a Diet Help Manage Diabetes?
Lifestyle and daily routine play a big part in blood sugar levels and diabetes management, especially nutrition. Whenever we eat, our bodies break down the food into glucose, a type of sugar. In those without type 2 diabetes, the hormone insulin helps sugar leave the blood and enter the cells, which gives the cells energy. In those with type 2 diabetes, the body doesn’t make or use insulin well, causing sugar to build up in the blood which results in the cells not getting enough energy.
A diet can help manage or prevent/delay type 2 diabetes in many different ways. Foods that are high in refined carbs and sugar should be avoided because they may increase blood sugar and insulin levels, which can lead to diabetes. Limiting those foods and choosing options that don’t cause blood sugar spikes can help to reduce that risk. Instead, eating a good balance of many foods from the major food groups and cutting calories can provide all of the vitamins and minerals that are needed; and a Mediterranean diet is a good way to accomplish that.
A study conducted in 2020 found that higher adherence to a Mediterranean diet was associated with a 19% lower risk of suffering from type 2 diabetes. The study highlighted the long-term protective effects of a Mediterranean diet, along with reducing the risk of heart disease. In fact, an analysis of more than 1.5 million healthy adults demonstrated that following a Mediterranean diet was associated with a reduced risk of death from heart disease and cancer, as well as a reduced incidence of Parkinson’s and Alzheimer’s diseases.
Research has also found that consumption of a Mediterranean-style diet by patients with metabolic syndrome is associated with improvement of endothelial function and a significant reduction of markers of systemic vascular inflammation. A Mediterranean-style diet has been found to be a safe strategy for treatment of the metabolic syndrome, which can be helpful in preventing type 2 diabetes since those with metabolic syndrome have a raised risk of developing diabetes.
How Can Physical Activity Help Manage Diabetes?
Another part of lifestyle that plays a big role in blood sugar levels and diabetes management is physical activity. Exercising regularly causes your muscles to use glucose for energy and your body to use insulin more efficiently. Both of these working together causes your blood sugar levels to lower.
The more difficult the workout is, the longer those effects will last. However, even light activities can improve blood sugar. While physical activity is a great way to manage diabetes and control blood sugar levels, there are also many more benefits it provides that can lower your risk of diabetes and other chronic diseases.
Regular physical activity can improve fitness level, cardiovascular health, and muscle tone, lower the risk of heart disease and nerve damage, promote sleep and relieve stress, release endorphins, cure diseases such as some forms of heart disease, cancer, help with arthritis, and even reverse depression, along with many more benefits.
What Are the Guidelines for This Plan?
The focus of the Mediterranean Diet isn’t on limiting total fat consumption, but rather on choosing healthier types of fat. This diet discourages saturated fats and hydrogenated oils (trans fats), both of which contribute to heart disease. It features olive oil as the primary source of fat; olive oil is mainly monounsaturated fat — a type of fat that can help reduce low-density lipoprotein (LDL) cholesterol levels when used in place of saturated or trans fats. “Extra-virgin” and “virgin” olive oils (the least processed forms) also contain the highest levels of protective plant compounds that provide antioxidant effects.
Canola oil and some nuts contain the beneficial linolenic acid (a type of omega-3 fatty acid) in addition to healthy unsaturated fat. Omega-3 fatty acids lower triglycerides, decrease blood clotting, and are associated with decreased incidence of sudden heart attacks, improve the health of your blood vessels, and help moderate blood pressure. Fatty fish — such as mackerel, lake trout, herring, sardines, albacore tuna and salmon — are rich sources of omega-3 fatty acids. Fish is eaten on a regular basis in the Mediterranean diet.
Although historically rich in grains, the Mediterranean diet is easily made gluten free for this plan! There are some specific steps to get your patients started:
1. Eat your veggies and fruits, and switch to whole grains.
A variety of plant foods should make up the majority of your meals. They should be minimally processed — fresh and whole are best. Include veggies and fruits in every meal and eat them for snacks as well.
2. Go nuts.
Nuts and seeds are good sources of fiber, protein and healthy fats. Keep almonds, cashews, pistachios and walnuts on hand for a quick snack.
3. Pass on the butter.
Try olive or canola oil as a healthy replacement for butter or margarine.
4. Spice it up.
Herbs and spices make food tasty and can stand in for salt and fat in recipes.
5. Go fish.
Eat fish at least twice a week. Fresh or water-packed tuna, salmon, trout, mackerel and herring are healthy choices. Grill, bake or broil fish for great taste and easy cleanup. Avoid breaded and fried fish.
6. Cut red meat out of your diet.
Substitute fish and poultry instead of red meat. Eating even small amounts of red meat have been shown to significantly increase the risk of type 2 diabetes. Also avoid sausage, bacon and other high-fat, processed meats.
7. Choose low-fat dairy.
Limit higher fat dairy products, such as whole or 2 percent milk, cheese and ice cream. Switch to skim milk, fat-free yogurt and low-fat cheese.
This plan can also be easily altered to suit the preferences and needs of your patients. If they are vegetarian, vegan, on a low-sodium diet, or on a low-fat diet, you can easily modify these plans for them.
What’s Inside the Plan?
Guiding your patients through new eating habits and lifestyles can be difficult, and it can definitely be a chore to collect all of the needed information.
Fortunately, their program will provide them with daily recipes, motivation, guidance, and tasks in order to help them transition to the Mediterranean Diet for Diabetes made specially for them. This way, they can maintain their healthy eating plan and blood sugar and diabetes management even after the 28 days are up.
Each day, their program will start with some helpful tips for blood sugar and diabetes management or heart health that they can follow throughout their everyday lives. Here is an example:

These are intended to keep your patients motivated to use these tips and ideas that will help them maintain a healthy lifestyle while managing their blood sugar and diabetes during and after the Mediterranean Diet for Diabetes Plan. Patients can take in the information provided and use it throughout their daily lives.
Their daily motivation or tips are then followed by daily tasks that will keep them on a healthy, grounded schedule throughout their plan. Here is an example:
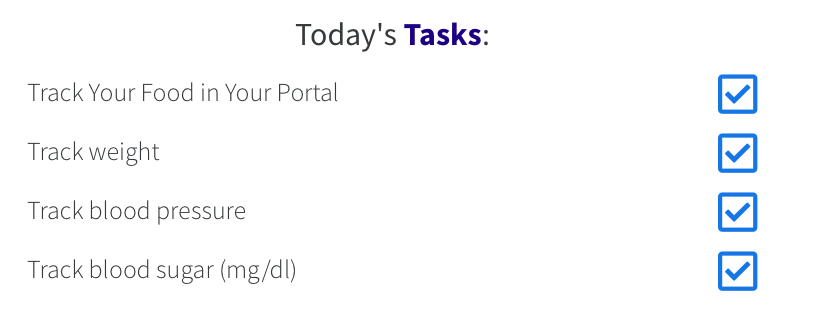
These tasks encourage patients to make sure they are tracking the food and metrics that need to be tracked in order to keep you updated with their progress.
Following these tasks are the daily recipes with instructions that your patients will follow. They are provided with a shopping list for each week so that they never miss a day of good meals. Here is an example:
Dinner
 Grilled Salmon with Shrimp
Grilled Salmon with Shrimp
Calories: 295 Total Fat: 19g Total Carbs: 1g Protein: 28g
Serves 1:
3 oz of salmon
2 oz of deveined, cleaned shrimp
2 tsp of extra virgin olive oil
Sea salt to taste if desired
Freshly ground pepper to taste
1 tbsp of chopped fresh thyme
1/4 tsp of dried hot red pepper flakes (optional)
1 tbsp of fresh lemon juice
2 tbsp of finely chopped parsley
Each day provides this content for your patients and are a great help when it comes to easily adjusting to their new lifestyle.
Why the Mediterranean Diet for Diabetes Plan?
We recognize that some doctors and some patients may need individualized approaches to wellness plans, so that’s why our Mediterranean Diet for Diabetes Plan as well as our 60+ other remote care programs are all customizable using out content management system, if you choose to modify the program.
Their program will also come with access to a complete remote patient monitoring web portal and app for iPhone and Android. Patients will be able to track their progress, keep a journal, and follow your prescribed program materials everyday with ease, all while making the process of health monitoring much easier for you.
Use the Mediterranean Diet for Diabetes Plan today to guide your patients through a practical heart-healthy eating plan that will help patients with blood sugar & diabetes management. If you’re not already using the BodySite remote care platform, you can sign up for a free trial at this link. If you’re already a member, check out the Mediterranean Diet for Diabetes today!
Disclaimer: The Mediterranean Diet for Diabetes Plan may not be sufficient to prevent, manage, or reverse type 2 diabetes. Patient outcomes may vary depending on the prescribing provider and individual situation of the patient.
SOURCES:
1. https://www.cdc.gov/diabetes/basics/type2.html
